Teamwork
Inspiring Beyond Borders – Grenada Global Partnership

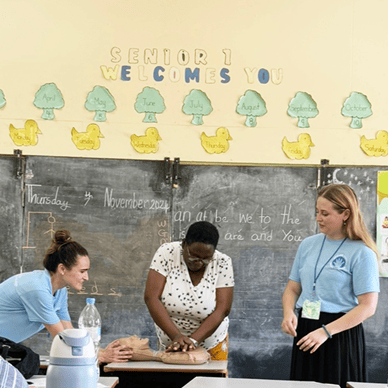
Grenada Global Partnership; Lurie Children's nurses travel to Grenada to provide hands-on training and educational sessions at St. George’s Hospital, Queen Elizabeth Home for Children (a local orphanage), Limes School (a special education school), and Dorothy Hopkin’s Home (a facility for individuals living with disabilities)
Lurie Children’s nurses are dedicated to the health and well-being of children not only in Chicago but around the world. In 2024, the Department of Nursing at Lurie Children's developed a Global Health Program, Healing Hands, bringing two groups of Lurie Children's nurses to Grenada in its inaugural year. This program’s mission is to provide pediatric nursing expertise to underserved communities while building cultural knowledge of self and others, engagement and purpose for Lurie Children’s nurses.
This initiative, made possible through philanthropy, provided nurses with an incredible opportunity to step beyond their daily roles, build global health knowledge, and engage in meaningful education for Grenadian caregivers. Unlike traditional medical missions focused on diagnosis and treatment, this trip emphasized building capacity for self-sustainment — empowering local caregivers with evidence-based practices to enhance patient care.
“This trip was truly inspiring, it motivated me to think beyond my day-to-day responsibilities and see the broader impact of nursing. Building relationships and trust with caregivers in Grenada was incredibly rewarding, and I’m excited for our nurses to continue supporting their community through education and collaboration.”
Kira Ziolkowski, BSN, RN, Medical Imaging Nursing Team (MINT)
Nurses provided hands-on training and educational sessions at St. George’s Hospital, Queen Elizabeth Home for Children (a local orphanage), Limes School (a special education school), and Dorothy Hopkin’s Home (a facility for individuals living with disabilities). They covered topics ranging from fetal circulation and CPR to skin care and caregiver-to-caregiver communication, adapting their teaching methods for caregivers with medical and non-medical backgrounds.
One of the most powerful takeaways was the universal need for well-being support for caregivers. Just as well-being has become a growing focus at Lurie Children’s, caregivers in Grenada expressed a strong desire to incorporate well-being practices into their daily care. “Sometimes, hearing from someone facing similar challenges is what truly highlights the need for support and well-being. It was eye-opening to realize that despite our differences, we share many of the same struggles,” Ziolkowski reflected.

Lurie Children's nurses Meghan Leshock, BSN, RN, CNOR, Operating Room (center) and Allison Schroepfer, MSN, RN, NI-BC, CPN, Nursing Informatics and Innovation (back, right)
CPR training; Lurie Children's nurses Amy O'Grady, BSN, RN, NICU (left) and Briana Meredith, BSN, RN, CPN, General Med/Pulmonary (right)
For the nurses, this opportunity was more than just a trip—it was a transformative experience. It reignited their passion, broadened their cultural awareness, and deepened their appreciation for the resources and education available at Lurie Children’s. It reinforced the power of knowledge-sharing and the profound, lasting impact that collaboration can have on global healthcare.
Transplant Nurse Coordinators:
Making Life-Saving Kidney Transplants Possible
In 2024, Lurie Children’s Pediatric Kidney Transplant Program led the nation in volumes, completing 44 transplants. This extraordinary feat was made possible thanks to selfless living organ donors, generous families of deceased donors and the demanding work of dozens of nursing, medical and surgical staff.
Being “Santa’s helper” is one way Kaitlyn White, BSN, RN, CPN, Nurse Coordinator, Division of Kidney Diseases, describes her role as an ambulatory nurse coordinator in the Kidney Transplant Program. The analogy speaks to the crucial role that she and her fellow nurse coordinator Katrina Andracki, BSN, RN, CPN, play in helping Santa (the medical and surgical teams) prepare for Christmas Day (transplantation).
Not one kidney transplant occurred in 2024 at Lurie Children’s without White and Andracki’s involvement. The duo coordinates pre-transplant care, ensuring patients receive necessary evaluations, medications and any needed follow-ups. They educate families, provide emotional support and bridge communication between specialists. Their expertise minimizes complications, enhances patient outcomes and improves quality of life for Lurie Children’s young patients.

Left to right: Alyssa Klehr, MD, RD, LDN, Clinical Nutrition, Kaitlin White, BSN, RN, CPN, CBC, Division of Kidney Diseases, Katrina Andracki, BSN, RN, CPN, Division of Kidney Diseases, and Allison Kozuch, BSN, RN, Division of Kidney Diseases
Recognizing the Kidney Transplant program’s growth and potential, White identified the need for an additional Nurse Coordinator to meet the program’s needs. White, who is a former inpatient nurse at Lurie Children’s, transitioned to her current role five years ago. Andracki filled in for White on an interim basis in 2023. Following the interim role fulfillment, White worked with Andracki to advocate for an additional, permanent role by gathering data to justify the additional position. With support from management, the request was approved, allowing both nurses to evaluate patients efficiently as well as contribute to kidney transplant research.
“Our amazing volumes and outcomes last year provide the best possible proof that having two of us in this position is worthwhile,” said White, referring to the 44 transplants done in 2024, compared to 26 the two prior years.
In addition to patient care, the duo works to help identify inefficiencies and implement process improvements in the kidney transplant process. One focus has been launching paired kidney exchange at Lurie Children’s. This involves swapping kidneys between donor-recipient pairs who aren't a match with each other but can match with another pair in a similar situation. This allows a recipient’s family to search for a living donor kidney transplant swap across the country who is also a great genetic match for their child, leading to a lower risk of rejection and graft failure.
Both nurses say they get great satisfaction from their non-traditional nursing jobs. The best part? Learning that a patient they worked with pre-transplant has an organ available.
“We work with these patients and families through some of their hardest days,” Andracki said. “Getting them to transplant is so rewarding.”
